My teenage daughter has Rett Syndrome and has always been served in a setting designed for individuals with autism. It has generally served her well, as she needs highly individualized care, and has responded well to ABA intervention. Over the years, her medical needs have grown more complex, and I am wondering about the best settings for her as she ages into adulthood. What should I be thinking about? What settings can manage both the behavioral and medical challenges she presents? How can families of individuals with Rett Syndrome plan for care as their child ages?
Answered by Emily Chin, PT, DPT and Mary Jane Weiss, PhD, BCBA-D
Melmark

Photographed by MART Production (pexels.com)
Thank you for your question. It is inspirational to see your advocacy in securing the right kinds of support as your daughter prepares to enter adulthood. Complex physical and behavioral needs present challenges to providers and can worry families making decisions about care. As such, it is important for these individuals to have access to specialized care that provides comprehensive assessment and individualized treatment.
Rett Syndrome
Rett Syndrome (RTT) is a genetic, complex, and progressive neurodevelopmental disorder with a wide range of physical and cognitive presentations (Sernheim et al., 2018; Rozensztrauch et al., 2021; Young et al., 2022). This disorder affects the brain development of almost exclusively girls and is associated with various comorbidities such as respiratory problems, scoliosis, epilepsy, malnutrition, and motor coordination challenges (Rozensztrauch et al., 2021; Young et al., 2022). As you are likely aware, regression or loss of previously learned skills is part of the disease progression. Deterioration in motor performance abilities includes the loss of purposeful hand movement, reduced ambulation (ability to walk), and increased stiffness. Provided the progressive nature of RTT and associated comorbidities with age, an interdisciplinary approach to care is imperative to maximize quality of life, safety, and independence (Fu, et al., 2022).
Individuals with RTT present with limitations in gross motor function, balance, strength, communication, safety awareness, emotional control, and cognition. This combination of needs limits their ability to navigate within the school, residential, and community environments independently (Fu, et al., 2022; Sernheim et al., 2018; Medline Plus, 2023). Accommodation and/or adaptive equipment are needed to ensure safety and promote independence across various activities of daily living and participation in educational and family life. Examples of adaptive equipment include gait belts/harnesses, gait trainers, modified seating, and/or shower safety equipment. Examples of accommodations may include the use of visual schedules, augmentative or alternative communication (AAC) systems, simplified communication approaches, and specialized teaching procedures. All these modifications require specific training for family members, caregivers, and teachers to ensure safe use and effectiveness across time, settings, people, and situations. Each discipline can provide a valued perspective to patient care and to caregiver education and training. Given the expected loss of skills, the team should be prepared to adapt treatments, accommodations, and equipment to the needs of the individual across the lifespan (Rozensztrauch et al., 2021; Medline Plus, 2023; Fonzo et al., 2020). These modifications are best achieved with consistency and cooperation of the interdisciplinary approach, along with continuous training. Given the benefits in treatment outcomes associated with interdisciplinary care, it is vital to create teams that represent these specialized skills from multiple disciplines (American Speech and Hearing Association, 2022; National Association for Rare Disorders, 2023). See Table 1 for a listing of team members involved in client care.
Case Illustration
Below we discuss the needs of an individual with Rett Syndrome, and review how an interdisciplinary approach guided the development of a comprehensive intervention. This may help illustrate intervention components that are needed to ensure comprehensive care.
The individual was an 18-year-old female with Rett Syndrome and a rare genetic disorder involving the MEPC2 gene, resulting in medically refectory epilepsy, a history of autistic features, a history of global developmental delay, inattention, constipation, sialorrhea (drooling), urinary retention, and a communication disorder. She was a multi-modal communicator and utilized an AAC device to clarify communication as needed to make all needs and wants known throughout her day. This individual attended a residential and school program where the primary methodology is applied behavior analysis. Across all settings, she was taught in a 1:1 staff-to-student ratio for skill acquisition and safety (due to medical comorbidities). In addition, she also received services in the areas of physical therapy, occupational therapy, and speech and language pathology.
Interdisciplinary Approach: Key Members
The nursing team provides insight as to how variables such as medication side effects or time of day medication is delivered might influence motor control, balance, and safety. The nurses also play a significant role in communication with other medical professionals (e.g., the neurologist, epidemiologist, cardiologist, and nutritionist).
-
- In this case study, nursing helped in assessing safety considerations. In addition to the regular monitoring by the physician and physical therapist, equipment was also needed to ensure safety. Specifically, the use of a padded hat and other safety equipment was established during times with a high probability of head drops. Ongoing knowledge of baseline levels of alertness and physical presentation is also important to the ability to reassess for changes related to any fall instability or seizure activity.
The occupational therapists (in collaboration with speech language pathologists) provide a valuable understanding of sitting position, swallowing strategies, and adaptive equipment that can be utilized to ensure safe meals. These therapists can assess and define what an individual’s readiness to eat may look like in terms of alertness, physical strength, and level of participation.
-
- For this case study, it was determined the student remained most safe when being dependently fed meals, and when food deliveries were paused to provide physical support during any instance of involuntary head drops (a decrease in motor control can lead to the loss of the ability to self-feed, as evident here). The occupational therapist provided expert advice as to how to maintain and practice grasping utensils without the daily practice of self-feeding (i.e., playing games that require grasping or pinching an item, carrying small items, and transferring with a spoon) as similar grasp is used for other functional tasks practiced less frequently than meals (i.e., coloring, tooth brushing). This level of practice is imperative while an individual progresses through stages of RTT in which purposeful hand movements may be lost and replaced with abnormal hand movements such as clasping, tapping, and hand wringing (Medline Plus, 2023).
Speech-language pathologists are experts in communication. Throughout all stages of RTT, the entire interdisciplinary team will need to consult on ways to incorporate the individual’s ability to communicate wants and needs and to adapt these strategies and systems as skills change.
-
- For this case study, the individual preferred to communicate vocally; however, she was often misunderstood by both familiar and novel communication partners. To supplement communication, an AAC device was initiated to repair communication breakdowns. Progress on learning to use the device has been slow but ongoing. The individual can repair requests for high-frequency items by using gestures as needed (i.e., books, food, and leisure items). Overall, the individual’s accuracy in communication is higher while sitting and with minimal environmental distractions.
The physical therapists’ role within the team is to establish protocols and guidelines for equipment that allow for maximal safety and functional independence with transitions and functional mobility (e.g., stair navigation, vehicle transfers, moving on and off different surfaces such as floors, chairs, and toilets). The physical therapist not only establishes the least restrictive type of equipment needed but constantly reassesses the need to fade or increase support based on changes in physical performance over time. Gross motor function continues to be affected throughout the lifespan and physical therapists can reduce or prevent limitations and improve their quality of life (Downs et al., 2017; Medline Plus, 2023; Young et al., 2022; Fonzo et al., 2020). It should be noted that approximately half of individuals with RTT can walk with assistance and maintaining this skill is crucial for independence (Young et al., 2022).
-
- For this case study, a gait harness, gait trainer, padded hat, shower chair, and modified chair (i.e., narrow seat with armrests) were identified (Please see Table 2 for links to the gait harness and padded hat.). Training is followed by frequent booster sessions and integrity checks, which are continuous across all areas of the school and residential base living. Booster sessions are provided in the settings where challenges have been noted and are often conducted by the occupational therapist or behavior analyst. Parent collaboration has also been a large component, both to ensure carryover in the home and to obtain all needed equipment through insurance.
Once all disciplines have established the accommodations required for an individual, collaboration with behavior analysts can help provide techniques and strategies to maximize the effectiveness of those accommodations. For example, completing preference assessments for reinforcement schedules is an important tool for success. Behavior analysts also assist the team in operationally defining behaviors, identifying methods for data collection across all areas of independent living, identifying effective prompt hierarchies, and documenting/reacting to medical events. With specific data collection, patterns or declines can be objectively documented and relayed to the corresponding team members for further assessment.
-
- In this case study, the behavior analyst also established protocols for unsafe behavior related to mobility. The student presented with wandering behavior. Wandering behavior was defined as anytime the individual engaged in minimally two steps that deviated from the end destination of a transition without requesting to do so. These attempts involved physical resistance that was not responsive to verbal redirection. The function of this behavior was hypothesized to be positive reinforcement in the form of access to preferred items/locations/people, and negative reinforcement in the form of delayed exposure to non-preferred locations/activities. With the use of functional communication training (i.e., requesting/pointing to an item prior to wandering without support, verbal communication of wants), the team maximized safety and enabled access to desired items in a safe manner.
Training as an Essential Component
All accommodations and recommendations by each member of the interdisciplinary team are only as effective as the training provided to each caregiver interacting with the individual. For this case study, the interdisciplinary team adopted the behavior skills training approach (Parsons et al., 2012). The respective team members developed training materials and guidelines for use with specific step-by-step directions, pictures, and rationales to support caregivers. Next, didactic training was completed with the focus on the rationale to increase staff awareness of severity and risks. Training role-plays were then completed with the trainer, as well as with the student. Each caregiver was required to demonstrate competency before independently using the equipment/accommodation with the individual. Competency was measured with the use of a feedback tool, in which 100% accuracy was required due to the severity of consequences (i.e., injury to the individual). Given the number of caregivers across settings, training was completed directly with supervisors, who then trained their supervisees. This training model increases efficiency and reduces the burden of training on primary trainers. Feedback tools were then completed as a form of quality checks to establish the need for retraining or drift from protocols.
Summary
While all individuals with developmental disabilities benefit from an interdisciplinary approach, some conditions require collaboration across disciplines to receive effective treatment. Rett Syndrome is a complex and degenerative neurological disorder that requires careful and continuous monitoring. Changes occur in neurological status, physical stamina, muscular strength, balance, and cognitive ability. As such, a careful process of assessment and intervention is needed to ensure safety and to protect the individual. In this case study, the nuanced needs of the individual were assessed continually, enabling an individualized and dynamic approach to treatment.
It is important for individuals with Rett Syndrome to have access to the expertise offered by each discipline, and for there to be adequate and systematic training to ensure that all caregivers are trained to criterion. This case study illustrates the possibilities that exist for individuals with complex needs to be served in community settings and underscores the need to include goals in safety maintenance, injury prevention, maintenance of physical functions, and continued skill acquisition for such learners.
Final Note and Some Questions about the Settings
We thank the reader for their question on planning for the future for their daughter with Rett Syndrome. Our response highlights the importance of setting and of support. The unique needs of Rett Syndrome require specialized care and the expertise of multiple, allied disciplines working together to effectively support the individual. Looking for a setting that is used to manage such complex presentations will be important.
-
- Ask questions about the complex medical needs of current clients. Does the setting view themselves as experts in managing the needs of individuals with complex medical and behavioral needs?
- Ask questions about the ways in which interdisciplinary teams work together in these settings. Are there regular meetings with the whole team? Are co-treatment sessions (where members of two disciplines work together to deliver services simultaneously) arranged as needed?
- Ask questions about safety protocols, the availability of safety equipment, and the expertise of the staff in understanding mobility challenges.
Table 1: The Team Serving the Client with Rett Syndrome
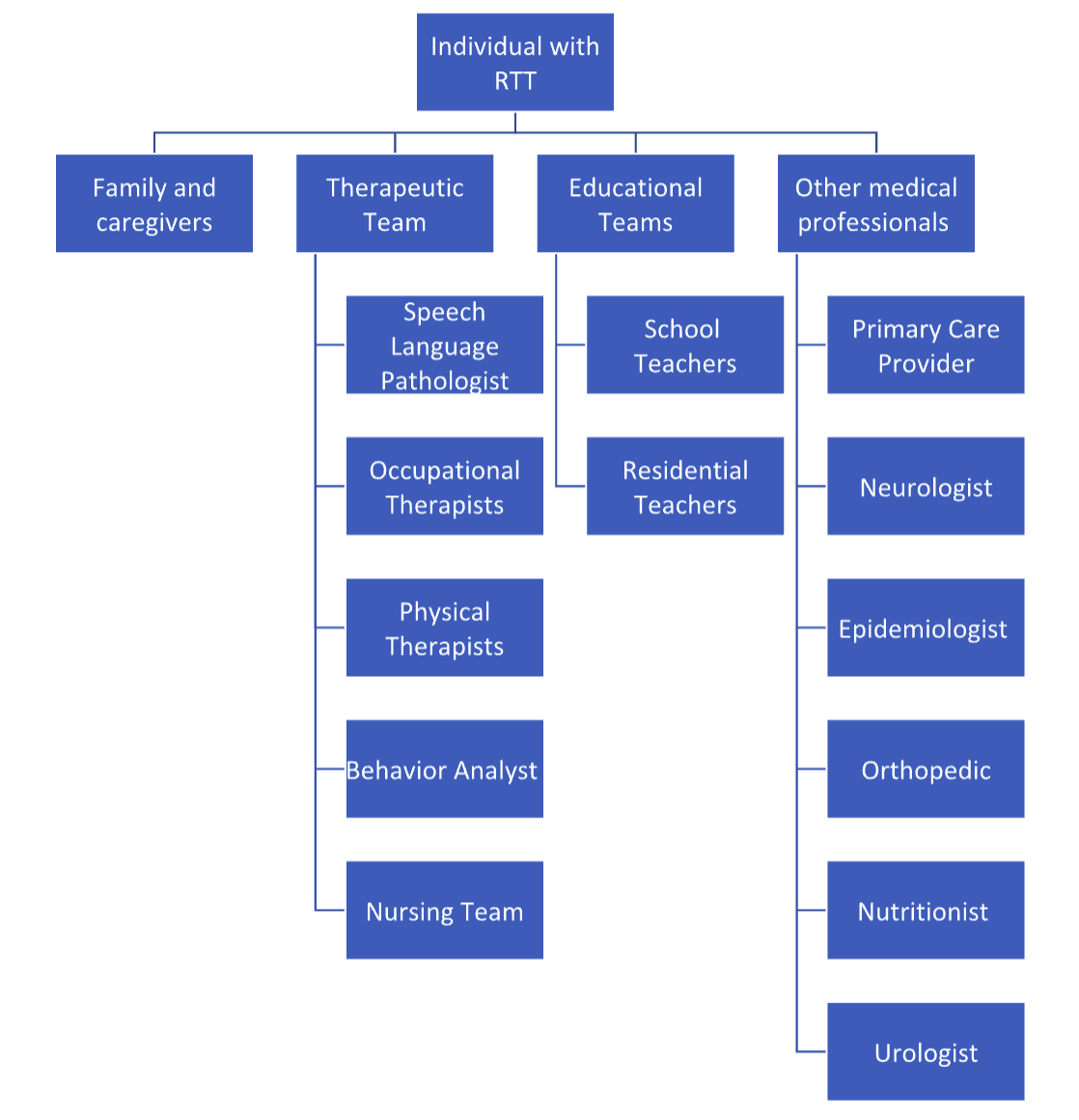
Table 2: Links to Equipment Utilized in this Case Study
| Equipment | Picture | Link |
| Gait Harness |  |
Drop Support Harness |
| Padded Hat |  |
RibCap Lenny Protective Hat |
Resources:
American Speech and Hearing Association. (2022) Joint Statement on interprofessional collaborative goals in school-based practice. https://www.asha.org/siteassets/ipp/joint-statement-on-interprofessional-collaborative-goals-in-school-based-practice-2022.pdf
Downs, J., Leonard, H., Wong, K., Newton, N., & Hill, K. (2017). Quantification of walking-based physical activity and sedentary time in individuals with Rett syndrome. Developmental Medicine and Child Neurology, 59, 605-611. https://doi.org/10.1111/dmcn.13398
Fonzo, M., Sirico, F., & Corrado, B. (2020). Evidence-based physical therapy for individuals with Rett Syndrome: A systematic review. Brain Science, 10(7):410. https://www.mdpi.com/2076-3425/10/7/410
Fu, C., Armstrong, D., Marsh, E., Lieberman, D., Motil, K., Witt, R., Standridge, S., Nues, P., Lane, J., Dinkel, T., Coenraads, M., von Hehn, J., Jones, M., Hale, K., Suter, B., Glaze, D., Neul, J., Percy, A., & Benke, T. (2020). Consensus guidelines on managing Rett syndrome across the lifespan. BMJ paediatrics open, 4(1), e000717. https://doi.org/10.1136/bmjpo-2020-000717
Medline Plus. (2023). Rett syndrome. Retrieved July 17, 2023, from https://medlineplus.gov/rettsyndrome.html
National Organization for Rare Disorders. [(accessed on 17 July 2023)]; Available online: https://rarediseases.org/rare-diseases/rett-syndrome/
Parsons, M. B., Rollyson, J. H., & Reid, D. H. (2012). Evidence-based staff training: A guide for practitioners. Behavior analysis in practice, 5, 2-11.
Rozensztrauch, A, Sebzda, A., & Śmigiel R. (2021). Clinical presentation of Rett syndrome in relation to quality of life and family functioning. Journal of International Medical Research, 49(4). https://doi.org/10.1177/03000605211007714
Sernheim, A., Hemmingsson, H., Witt Engerström, I., & Liedberg, G. (2018). Activities that girls and women with Rett syndrome liked or did not like to do. Scandinavian Journal of Occupational Therapy, 25(4), 267-277, https://doi.org/10.1080/11038128.2016.1250812
Young, D., Suter, B., Levine, J., Glaze, D., & Layne, C. (2022) Characteristic behaviors associated with gait of individuals with Rett syndrome, Disability and Rehabilitation, 44(8), 1508-1515, https://doi.org/10.1080/09638288.2020.1820084
Citation for this article:
Chin, E., & Weiss, M. J. (2024). Clinical Corner: How can families of individuals with Rett Syndrome plan for care as their child ages? Science in Autism Treatment, 21(2).
Other Related Clinical Corner Articles:
- Clinical Corner: Transition planning as it relates to challenging behaviors: Matching the individual to the right setting for adult services
- Clinical Corner: What is the relationship between autism spectrum disorders and intellectual disability?
- Clinical Corner: Catatonia in autism spectrum disorder
- Clinical Corner: What about maintenance programs?
- Clinical Corner: What are some considerations surrounding the initiation and fading of gastrostomy tubes?
- Clinical Corner: What is the importance of engagement when working with individuals with intellectual and developmental disabilities and autism?
- Clinical Corner: How can health informatics support our work?
- Clinical Corner: Reducing constipation medications in clients with intellectual disabilities
- Clinical Corner: Can psychotropic medications be safely reduced?
Related ASAT Interviews and Perspective Pieces:
- Interview with Eileen Lamb, mother and advocate
- Interview with Rita Gardner
- Interview with Purnima Hernandez, DDS, MA, BCBA
- The transition to adult services: Two parents’ journeys
- Jack matters, too: A mother’s perspective on her son’s place in the autism community
Related ASAT Articles:
- Treatment Summary: Augmentative and Alternative Communication (AAC)
- A non-exhaustive list of safety products
- Review of Life journey through autism: A guide to safety
- Changes to the DSM autism diagnostic criteria
- A review of Identification, evaluation, and management of children with autism spectrum disorder (Part 1 of 2)
- A review of Identification, evaluation, and management of children with autism spectrum disorder (Part 2 of 2)
- Description of the treatment team
- Focus on the treatment team: Occupational therapy
- Focus on the treatment team: Physical therapy
- Focus on the treatment team: Speech-language therapy
- Focus on the treatment team: Applied behavior analysis
- Media Watch: ASAT Responds to Psychologytoday.com’s Making severe autism visible
#Adolescents #MedicalProviders #Multidisciplinary #Residential